Blog
Understanding Ganglion Cysts on the Feet
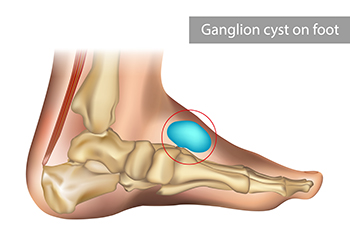
Ganglion cysts are fluid-filled lumps that commonly form along tendons or joints, including on the feet. These non-cancerous cysts vary in size and can sometimes cause discomfort, especially if located in areas that bear weight or experience friction from shoes. While the exact cause of ganglion cysts remains unclear, repetitive stress on the foot joints or trauma may contribute to their development. Symptoms range from a visible lump to pain, limited movement, and, in some cases, numbness if the cyst presses on nearby nerves. While ganglion cysts are generally harmless, treatment may be necessary if they cause discomfort or impede movement. Treatment options include draining the fluid, or, in more persistent cases, surgical removal. If you have this type of cyst, it is suggested that you visit a podiatrist for an exam and monitoring.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flat Feet in Children

Flat feet in children occur when the arches of the feet do not develop as expected, causing the entire foot to touch the ground. Some children outgrow flat feet as their muscles and bones strengthen, while others may develop persistent issues. Causes include having a tight Achilles tendon, tarsal coalition where foot bones fuse, and rigid flat feet that do not change with movement. A podiatrist can assess foot structure, recommend stretching exercises, orthotics, or treatment to improve comfort and prevent future problems. If your child has pain or difficulty walking from having flat feet, it is suggested that you promptly consult a podiatrist who can offer effective treatment relief and treatment solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Understanding Bunions and When Surgery May Be Needed

A bunion is a bony bump that forms on the joint at the base of the big toe, as the top of the toe leans inward. It may appear red, swollen, and feel painful or stiff, especially when walking or wearing tight shoes. Common causes include inherited foot structure, arthritis, or wearing narrow footwear. Symptoms range from mild discomfort to persistent pain, limited movement, and visible deformity. A podiatrist can diagnose a bunion through a physical exam and X-rays. Non-surgical treatments include custom orthotics, padding, anti-inflammatory medication, or shoe modifications to relieve pressure. If conservative methods fail and pain interferes with daily life, surgery may be considered. Surgical benefits include pain relief and improved foot alignment, but risks may include infection, nerve damage, or a lengthy recovery. Every case is unique, and a podiatrist can help determine the best course of action. It is suggested that you make an appointment with a podiatrist for proper evaluation and care.
If you are suffering from bunion pain, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors and Symptoms of Gout

Gout is a form of arthritis caused by a buildup of uric acid crystals in the joints, often affecting the big toe. It can lead to sudden pain, swelling, redness, and tenderness that makes walking difficult. Risk factors include genetic predisposition, diets rich in red meat or seafood, obesity, alcohol consumption, and underlying medical conditions such as kidney disease or hypertension. Symptoms range from intense joint pain to lingering discomfort and limited mobility. A podiatrist can provide a diagnosis, treatment, and guidance to prevent flare-ups while protecting joint health. If you have intense pain in your big toe, it is strongly suggested that you are under the care of a podiatrist who can help you manage this painful condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors and Symptoms of Athlete’s Foot

Athlete’s foot, also called tinea pedis, is a fungal infection that affects the skin of the feet. It can involve the spaces between the toes, the soles, or the heels. Symptoms of athlete's foot include peeling, cracked, or scaly skin between the toes, blisters filled with fluid, burning sensations, and itching. In some cases, a musty odor is present. The infection thrives in warm, damp conditions, making people who sweat heavily or wear tight, enclosed shoes for long periods more prone to it. Walking barefoot in public showers, around pools, or locker rooms, as well as sharing footwear, can also increase the risk of athlete’s foot. Older adults, men, people with diabetes, or those with weakened immune systems are more likely to develop this condition. A podiatrist can diagnose the infected area, provide treatment, and help prevent it from spreading to toenails or other areas. If you have symptoms of an athlete's foot infection, it is suggested that you make an appointment with a podiatrist for an evaluation and treatment.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Exercises That Can Help With Plantar Fasciitis

Plantar fasciitis is one of the most common causes of heel pain. Exercises that focus on the foot and ankle can help reduce discomfort and promote healing. The plantar fascia is a band of tissue that supports the arch of the foot, and when it becomes inflamed, pain often develops along the heel and sole. Stretching exercises that lengthen the calf muscles and the bottom of the foot may reduce stress on the plantar fascia. Strengthening exercises improve support and stability during walking. Movements that target the toes, such as pulling them gently back toward the ankle, can decrease tension across the arch. Strengthening the small muscles within the foot can also improve balance and lessen the load on the fascia. A podiatrist can assess the severity of plantar fasciitis, recommend safe exercises, and develop a treatment plan that may also include other supportive options. If you experience pain from plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist for treatment options, including exercises.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctors to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Managing Toenail Fungus

Nail fungus, also known as onychomycosis, affects the toenails, causing them to become thick, discolored, brittle, and sometimes foul-smelling. It often begins as a white or yellow spot under the nail and can spread deeper, causing the nail to darken, crumble, or even separate from the nail bed. Causes include exposure to moist environments, walking barefoot in communal areas like around pools or in gyms, wearing tight shoes, having athlete’s foot, or a weakened immune system. People with diabetes or poor circulation are also at a higher risk. In some cases, the infection may cause discomfort or pain, especially when wearing shoes. A podiatrist can diagnose nail fungus by examining the nail, and possibly taking a sample to confirm the type of fungus. Treatment options include topical or oral antifungal medications, or, in severe cases, removal of the affected nail. If you have toenail fungus, it is suggested that you schedule an appointment with a podiatrist for effective treatment solutions.
For more information about treatment, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing With Drop Foot

Drop foot, often called foot drop, is a condition where the foot cannot properly lift at the ankle, making it difficult to clear the ground while walking. This problem arises when the muscles at the front of the leg that control ankle motion become weak or lose function, or when the nerve supplying those muscles is damaged. People with drop foot may develop a high-stepping gait to avoid tripping, and without proper care, the ankle can stiffen into a downward pointing position. A podiatrist can evaluate the severity and underlying cause, and provide treatment to help restore mobility and function. Options include the use of an ankle-foot brace to keep the foot in a neutral position or surgery, such as tendon transfer or nerve repair, if the weakness is permanent. These treatments are designed to improve stability, walking ability, and reduce the risk of falls. If you have trouble lifting your feet when walking, it is suggested that you make an appointment with a podiatrist for treatment options.
If you have any concerns about your feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.