Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
First Aid for Ankle Sprains
Though it often affects athletes, an ankle sprain can happen to anyone, anytime, and anywhere. Sometimes all it takes to sprain an ankle is to land awkwardly after a jump, or twist your ankle too much as you step off a curb. Symptoms of an ankle sprain include pain in the ankle, particularly when trying to move it or put weight on it, and swelling. If you are feeling these symptoms following an injury, stop what you are doing and rest the affected ankle. Use ice packs wrapped in a towel and elevate your injured ankle to reduce swelling. You can also compress the ankle by wrapping it with an elastic bandage. A sprained ankle needs to heal fully and properly to avoid re-injury. If you have sprained your ankle, it is strongly suggested that you seek the care of a podiatrist.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Wounds That Don't Heal Need to Be Checked
What Do Orthotics Do?
 Shoe inserts that are designed to relieve pain caused by various foot conditions are known as orthotics. Common foot conditions treated by orthotics may include corns and calluses, tendonitis, bunions, heel pain, and stress fractures. Orthotics can also help non-foot related issues such as correcting posture and alignment. Orthotics come in a variety of types, including custom made ones, cushioned ones that absorb shock, and pressure relieving orthotics that distribute body weight across the sole of the foot. A podiatrist will consider many factors when prescribing orthotics, which include any existing foot conditions, the structure of the foot, biomechanics, and the patient’s lifestyle. If you believe that orthotics are right for you, a podiatrist will be able to help point you in the right direction.
Shoe inserts that are designed to relieve pain caused by various foot conditions are known as orthotics. Common foot conditions treated by orthotics may include corns and calluses, tendonitis, bunions, heel pain, and stress fractures. Orthotics can also help non-foot related issues such as correcting posture and alignment. Orthotics come in a variety of types, including custom made ones, cushioned ones that absorb shock, and pressure relieving orthotics that distribute body weight across the sole of the foot. A podiatrist will consider many factors when prescribing orthotics, which include any existing foot conditions, the structure of the foot, biomechanics, and the patient’s lifestyle. If you believe that orthotics are right for you, a podiatrist will be able to help point you in the right direction.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
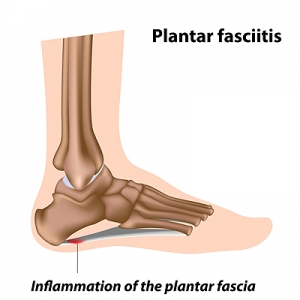
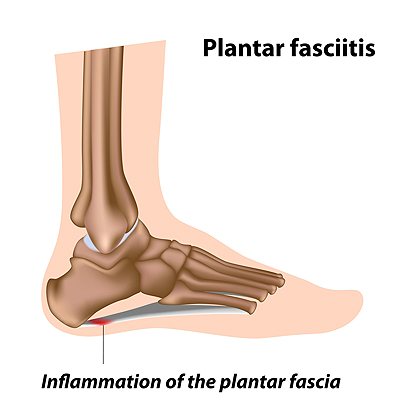
Why Do I Have Plantar Fasciitis?
Plantar fasciitis, the inflammation of the ligament that runs along the bottom of the foot and connects the toes to the heel bone, is a common cause of heel pain. When the plantar fascia is injured through repetitive strain, excessive exercise, prolonged standing, wearing uncomfortable shoes, or obesity, it may lead to stabbing heel pain that is typically at its worst when taking the first few steps after a long rest. Other possible causes of plantar fasciitis include structural abnormalities in the foot, such as having flat feet, high arches, overpronation, or leg length differences. Foot changes associated with aging or pregnancy may also be to blame in some cases. If you are suffering from heel pain, don’t hesitate to schedule an appointment with a podiatrist near you.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
The Importance of Foot Care For Diabetics
 Neuropathy, a form of nerve damage, is known for causing a loss of feeling in the feet, and roughly half of all diabetic patients have some type of neuropathy. Because of this lack of feeling, many small problems with the feet may not be noticed and thus lead to the development of serious issues. To help avoid missing the small issues that can occur with the feet, there are some daily things that diabetic patients can do. Daily checks for cuts and wounds, regularly washing the feet, wearing shoes that fit right, and avoiding going barefoot are a few of the things that can be done to help care for the feet once they have lost some feeling. Along with regular checkups, diabetic patients should consult with a podiatrist if they notice a loss of sensation in the feet, a change in shape or color to the feet, or loss of hair on the feet.
Neuropathy, a form of nerve damage, is known for causing a loss of feeling in the feet, and roughly half of all diabetic patients have some type of neuropathy. Because of this lack of feeling, many small problems with the feet may not be noticed and thus lead to the development of serious issues. To help avoid missing the small issues that can occur with the feet, there are some daily things that diabetic patients can do. Daily checks for cuts and wounds, regularly washing the feet, wearing shoes that fit right, and avoiding going barefoot are a few of the things that can be done to help care for the feet once they have lost some feeling. Along with regular checkups, diabetic patients should consult with a podiatrist if they notice a loss of sensation in the feet, a change in shape or color to the feet, or loss of hair on the feet.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.