Understanding Morton’s Neuroma
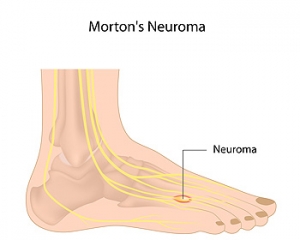
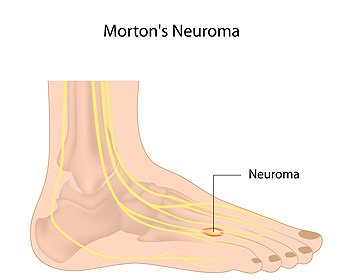
A neuroma is a condition where the tissue that surrounds a nerve becomes thickened and inflamed. A neuroma can materialize around any nerve of the body, but when it occurs between the 3rd and 4th toes (or less commonly the 2nd and 3rd toes), it is known as Morton’s Neuroma. This benign growth of nerve cells can cause tingling, pain, and numbness in the ball of the foot—often making it feel as if there is a pebble stuck in your shoe. It is suggested that you see a podiatrist if you suspect you have Mortaon’s neuroma, as the condition may worsen and possibly lead to permanent nerve damage.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. James Kutchback of James Kutchback, DPM, ABLES, CWS-P. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Should I Treat My Bunions?
 Bunions are bony growths that appear on the outer side of the foot at the base of the big toe joint. This is a deformity that may cause pain, swelling, redness, and difficulty wearing shoes and while walking. When left untreated, bunions tend to progressively worsen over time. As a bunion grows, it pushes the big toe towards the smaller toes, changing the shape of the foot in the process. The misaligned big toe may then push the second toe out of alignment. Bunions can also lead to arthritis in the big toe joints. Bunions can be managed and their progression can be slowed through a variety of conservative treatments, such as footwear modifications. Surgery may also be an option and can permanently correct a bunion. If you suffer from bunions, it is suggested that you see a podiatrist for treatment.
Bunions are bony growths that appear on the outer side of the foot at the base of the big toe joint. This is a deformity that may cause pain, swelling, redness, and difficulty wearing shoes and while walking. When left untreated, bunions tend to progressively worsen over time. As a bunion grows, it pushes the big toe towards the smaller toes, changing the shape of the foot in the process. The misaligned big toe may then push the second toe out of alignment. Bunions can also lead to arthritis in the big toe joints. Bunions can be managed and their progression can be slowed through a variety of conservative treatments, such as footwear modifications. Surgery may also be an option and can permanently correct a bunion. If you suffer from bunions, it is suggested that you see a podiatrist for treatment.
If you are suffering from bunions, contact Dr. James Kutchback of James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Arthritis Can Cause Pain in the Feet and Ankles
Athlete’s Foot: Not Just for Athletes
Athlete’s Foot is a fungal infection that affects the skin on the feet. Despite its name, this fungal infection does not only occur in athletes. In fact, Athlete’s foot affects 1 out of 10 Americans. Athlete’s Foot is also known as dermatophytosis of the foot or tinea pedis. The fungi that are responsible for this condition feed on skin proteins called keratin, and love hot and steamy environments such as locker rooms, swimming pools, non-breathable footwear, and blisters and cuts on the feet which allow them access into your system. Getting a proper diagnosis is important in order for your podiatrist to rule out other conditions such as eczema and psoriasis, and to provide proper treatment.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
When to Consult With a Podiatrist
 The foot is composed of 26 bones along with a variety of joints, tendons, ligaments and muscles. A podiatrist is a doctor that specializes in conditions that impact these structures of the foot as well as the ankle. They can specialize in a variety of specific areas, such as surgery, wound care, sports injuries, and diabetic conditions. Podiatrists can treat a variety of conditions that include (but are not limited to) bunions, heel pain, flat feet, sprains, warts, nail conditions, and corns or calluses. Podiatrists should be consulted when there is severe foot pain, swelling, numbness, an open sore or a sign of infection that lasts multiple days. You should also consult with a podiatrist immediately if the foot or ankle cannot bear any weight.
The foot is composed of 26 bones along with a variety of joints, tendons, ligaments and muscles. A podiatrist is a doctor that specializes in conditions that impact these structures of the foot as well as the ankle. They can specialize in a variety of specific areas, such as surgery, wound care, sports injuries, and diabetic conditions. Podiatrists can treat a variety of conditions that include (but are not limited to) bunions, heel pain, flat feet, sprains, warts, nail conditions, and corns or calluses. Podiatrists should be consulted when there is severe foot pain, swelling, numbness, an open sore or a sign of infection that lasts multiple days. You should also consult with a podiatrist immediately if the foot or ankle cannot bear any weight.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.