Items filtered by date: June 2024
Plantar Fibroma
A plantar fibroma is a knot in the arch of the foot. It can cause pain when repeated pressure is applied by walking barefoot or wearing tight shoes. While plantar fibromas can appear in anyone, men who are middle-aged or older are said to be more susceptible. The main symptom of a plantar fibroma is a firm lump on the arch of the foot. If there is pain, it can be intensified by putting pressure on the nodule. The lump can stay one size or grow larger. You may have one or more fibromas in the feet and there tends to be a high incidence of recurring plantar fibromas. Generally, a plantar fibroma can be treated without surgery. Treatment might include steroid injections to help shrink the lump, orthotics to help redistribute weight away from the nodule, plantar fascia stretching, or physical therapy to help use anti-inflammatory medication on the lump. If a lump grows larger or more painful, a podiatrist can be consulted to confirm the diagnosis. The doctor will palpate the lump and this may cause pain that can be felt all the way to the toes. An X-ray, MRI, or biopsy might be done if further evaluation is necessary. A lump in the arch of the foot might be something other than a plantar fibroma, such as cysts, nerve or fatty tumors, swollen tendons, or an infection in the foot. It is important to see a podiatrist for proper diagnosis and treatment of plantar fibromas.
Plantar Fibromas and Nonsurgical Relief Options

A plantar fibroma is a benign, fibrous knot embedded in the plantar fascia, the tissue along the bottom of the foot. This condition often causes a noticeable lump in the arch of the foot, leading to discomfort or pain when walking or standing. Nonsurgical relief options for plantar fibromas focus on reducing symptoms and improving foot function. Orthotic devices such as shoe inserts can help by distributing pressure more evenly across the foot and reducing strain on the plantar fascia. Stretching exercises and massage can alleviate tension and improve flexibility in the foot. Additionally, corticosteroid injections may be administered to reduce inflammation and pain associated with the fibroma. If you have developed a knot in the arch of your foot, it is suggested that you speak with a podiatrist who can determine what the best course of treatment is for you.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Causes and Diagnosis of Peripheral Artery Disease
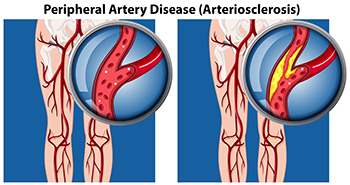
Peripheral artery disease, or PAD, poses significant challenges for foot health, stemming from restricted blood flow to the lower extremities. This condition, often caused by atherosclerosis, involves the buildup of fatty deposits in the arteries, leading to narrowed or blocked blood vessels. The diminished blood supply to the feet can result in various symptoms, including pain, cramping, numbness, and weakness, particularly during physical activity. Left untreated, PAD can contribute to serious complications such as foot ulcers, infections, and delayed wound healing. Diagnosing PAD typically involves a comprehensive evaluation by a podiatrist. This process includes a thorough medical history review, assessment of risk factors such as smoking and diabetes, and a physical examination focused on evaluating circulation in the legs and feet. Specialized diagnostic tests, such as ankle-brachial index, or ABI measurement, Doppler ultrasound, and angiography, may also be employed to confirm the diagnosis and determine the extent of arterial blockages. If you are experiencing any of the foot symptoms mentioned above, it is suggested that you consult a podiatrist who can accurately diagnose and offer relief solutions for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Poor Circulation in Your Feet
 Are your feet frequently cold or numb? If so, you may be experiencing poor circulation, a condition that affects blood flow to the feet. Poor circulation can lead to a range of uncomfortable symptoms, including cold feet, numbness, tingling sensations, and sometimes slowly healing wounds. This condition is often caused by underlying health issues such as diabetes, peripheral artery disease, or vascular problems. Ignoring poor circulation can lead to serious complications, including tissue damage and infections. Don't let poor circulation hold you back from enjoying life. If you are experiencing poor circulation in your feet, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options and prevent any further complications or discomfort.
Are your feet frequently cold or numb? If so, you may be experiencing poor circulation, a condition that affects blood flow to the feet. Poor circulation can lead to a range of uncomfortable symptoms, including cold feet, numbness, tingling sensations, and sometimes slowly healing wounds. This condition is often caused by underlying health issues such as diabetes, peripheral artery disease, or vascular problems. Ignoring poor circulation can lead to serious complications, including tissue damage and infections. Don't let poor circulation hold you back from enjoying life. If you are experiencing poor circulation in your feet, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options and prevent any further complications or discomfort.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
Surgical Excision of a Plantar Fibroma

Plantar fibromas are benign growths that develop in the arch of the foot, often causing discomfort and difficulty with walking. When conservative treatments fail to provide relief, foot surgery may be necessary to alleviate symptoms and restore mobility. During the procedure, the patient is typically placed under local anesthesia, numbing the foot to minimize pain. The surgeon then makes an incision in the skin, carefully dissecting the fibroma from surrounding tissues and nerves. Once the fibroma is removed, the incision is closed with sutures, and a dressing is applied to promote healing. Recovery time varies, depending on the size of the fibroma and the individual's ability to heal, but most patients can expect to resume normal activities within a few weeks. While surgical plantar fibroma excision offers a permanent solution, it is essential to discuss the risks and benefits with a podiatrist. If you have a plantar fibroma that is causing you pain, it is suggested that you make an appointment with a podiatrist who can determine if this surgery is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.